The Challenge
Around the world today, many countries still don’t accurately count and classify who is born, who dies, and other important details about people’s health throughout the years in-between. Moreover, the health data that is available is often fragmented and incomplete, with multiple stakeholders reporting the same information using different methods and through different channels.
That makes it harder for administrators and policy-makers to make evidence-based decisions about where to target resources that can improve well-being and help people to live longer, healthier and more productive lives.
The Health Data Collaborative addresses those challenges by supporting global health partners to align their financial and technical resources around a common agenda for measurement and accountability.
Below are some of the barriers to consistently using data to inform action.
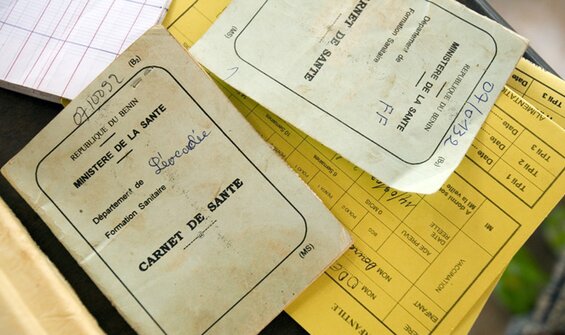
Inadequate civil registration and gaps in vital statistics
Civil registration and vital statistics (CRVS) systems are implemented by governments to register all births, deaths and causes of death; however, their governance, accountability, implementation and capacity differ greatly between countries. As such, the completeness and availability of CRVS data also varies. For example, a survey of 133 country health information systems conducted between 2018 and 2020 found that 4 in 10 deaths globally are not registered, with this number rising to 9 in 10 deaths in Africa. In addition, 77 countries were found not to produce any cause-of-death data at all. The COVID-19 pandemic has revealed the true extent of these gaps and was a tragic reminder of our inability to fully account for all of the lives lost and lives affected, either directly or indirectly.
This is not just a statistical barrier - it’s also a human rights barrier. Without this foundational data, countries are unable to measure the impact of public health policies. It also presents the risk that some people will be left behind, unable to prove their legal identity and claim their right of access to public services. This is particularly true for migrants, refugees and stateless populations, which have increased greatly in recent years.
The HDC response:
Civil Registration and Vital Statistics working group
Irregular reporting and non-standardised health indicators
Health facilities generate data on an ongoing basis during the course of their service delivery, but many countries face challenges in reporting this data and converting it into meaningful actions. These challenges may include high-volume data demands, poor quality data, infrequent or delayed reporting, inadequate feedback mechanisms, and insufficient infrastructure or human resources.
Non-standardised indicators of heath also complicate health reporting at an aggregate level. Health indicators - such as those used to measure progress towards SDG3 on health and well-being - are the measurable characteristics used to assess the health of a population over time and space.But how are these defined? Mortality and fertility status, environmental risk factors, disease-specific service coverage, and health systems quality all need to be considered when assessing population health. These indicators should also be disaggregated by key equity stratifiers such as age, sex, income, and geographic location to get a more accurate picture of the state of a population’s health.
However, the availability of this data by indicator varies widely, both in terms of availability and quality. For example, while 100% of countries had recent underlying data to estimate air pollution in 2020, only 9% were able to measure access to essential medicines - another area that was exacerbated during COVID-19.
The HDC response:
Community Data working group
Routine Health Information Systems working group
Fragmented technologies and digital data risks
Health data is generated across a myriad of care settings, organizations and geographies, with each utilizing different IT systems and standards to do so. One of the biggest challenges in using health data to optimize patient outcomes is enabling digital data to flow securely between different systems - what is often referred to as ‘interoperability’. Health information systems and devices must become interoperable to work across organizational and national boundaries, ensuring that solutions are also sustainable for low and middle income countries that may still largely rely on, for example, on mobile phone technology or in-person surveys.
At an individual and institutional level, there can be a natural reluctance to share health data due to its personal and sensitive nature. As health technologies continue to advance and more of our data becomes available in a digital format, it will be essential to increase awareness of the direct benefits of sharing health data with the reassurance that this can be done according to best practices for data privacy, protection and security..
The HDC response:
Digital Health & Interoperability working group
Data and Digital Governance working group